If You Have been diagnosed or may have Prostate Cancer
Rio Grande Cancer Foundation
Call us:
M-F: 8AM - 5PM | Sat-Sun: Closed
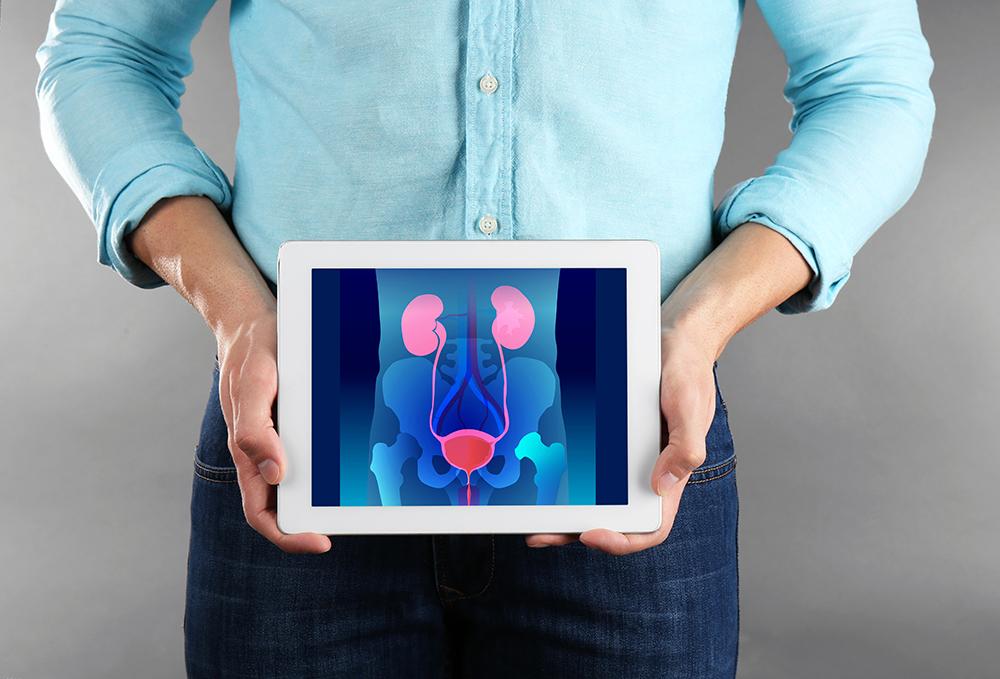
Prostate cancer begins when cells in the prostate gland start to grow out of control. The prostate is a gland found only in males. It makes some of the fluid that is part of semen. The prostate is below the bladder (the hollow organ where urine is stored) and in front of the rectum (the last part of the intestines). Just behind the prostate are glands called seminal vesicles that make most of the fluid for semen. The urethra, which is the tube that carries urine and semen out of the body through the penis, goes through the center of the prostate. The size of the prostate can change as a man ages. In younger men, it is about the size of a walnut, but it can be much larger in older men.
Types:
Almost all prostate cancers are adenocarcinomas. These cancers develop from the gland cells (the cells that make the prostate fluid that is added to the semen).
Other types of cancer that can start in the prostate include:
- Small cell carcinomas
- Neuroendocrine tumors (other than small cell carcinomas)
- Transitional cell carcinomas
- Sarcomas
These other types of prostate cancer are rare. If you are told you have prostate cancer, it is almost certain to be an adenocarcinoma.
Some prostate cancers grow and spread quickly, but most grow slowly. In fact, autopsy studies show that many older men (and even some younger men) who died of other causes also had prostate cancer that never affected them during their lives. In many cases, neither they nor their doctors even knew they had it.
Tests:
The PSA test can also be useful if you have already been diagnosed with prostate cancer.
In men just diagnosed with prostate cancer, the PSA level can be used together with physical exam results and tumor grade (determined on the biopsy, described further on) to help decide if other tests (such as CT scans or bone scans) are needed.
The PSA level is used to help determine the stage of your cancer. This can affect your treatment options, since some treatments (such as surgery and radiation) are not likely to be helpful if the cancer has spread to other parts of the body.
PSA tests are often an important part of determining how well treatment is working, as well as in watching for a possible recurrence of the cancer after treatment (see Following PSA Levels During and After Treatment).
Prostate biopsy
If the results of a PSA blood test, DRE, or other tests suggest that you might have prostate cancer, you will most likely need a prostate biopsy.
A biopsy is a procedure in which small samples of the prostate are removed and then looked at with a microscope. A core needle biopsy is the main method used to diagnose prostate cancer. It is usually done by a urologist. During the biopsy, the doctor usually looks at the prostate with an imaging test such as transrectal ultrasound (TRUS) or MRI, or a ‘fusion’ of the two (all discussed below). The doctor quickly inserts a thin, hollow needle into the prostate. This is done either through the wall of the rectum (a transrectal biopsy) or through the skin between the scrotum and anus (a transperineal biopsy). When the needle is pulled out it removes a small cylinder (core) of prostate tissue. This is repeated several times. Most often the doctor will take about 12 core samples from different parts of the prostate.
Though the procedure sounds painful, each biopsy usually causes only some brief discomfort because it is done with a special spring-loaded biopsy instrument.
Understanding your stage:
The following clinical stages are used to describe prostate cancer:
• T1: The tumor cannot be felt during the DRE or seen during imaging (e.g., a computed tomography (CT) scan or transrectal ultrasound). It may be found when surgery is done for another medical condition.
T1a: The tumor is discovered accidentally during a surgical procedure used to treat benign prostatic hyperplasia (BPH), which is the abnormal growth of benign prostate cells. Cancer is only found in 5 percent or less of the tissue removed.
T1b: The tumor is found accidentally during BPH surgery. Cancer cells are detected in more than 5 percent of the tissue removed.
T1c: The tumor is found during a needle biopsy that was performed because of an elevated PSA level.
• T2: The tumor appears to be confined to the prostate. Due to the size of the tumor, the doctor can feel it during the DRE. The cancer may also be seen with imaging.
T2a: The tumor has invaded one-half (or less) of one side of the prostate.
T2b: The tumor has spread to more than one-half of one side of the prostate, but not to both sides.
T2c: The cancer has invaded both sides of the prostate.
• T3: The tumor has grown outside the prostate. It may have spread to the seminal vesicles.
T3a: The tumor has developed outside the prostate; however, it has not spread to the seminal vesicles.
T3b: The tumor has spread to the seminal vesicles.
• T4: The tumor has spread to tissues next to the prostate other than the seminal vesicles. For example, the cancer may be growing in the rectum, bladder, urethral sphincter (muscle that controls urination) and/or pelvic wall.
Treatment:
What kind of treatment will I need?
Because most prostate cancers are found in the early stages when they are growing slowly, you usually do not have to rush to make treatment decisions. During this time, it is important to talk with your doctor about the risks and benefits of all your treatment options and when treatment should begin.
• Active surveillance and watchful waiting
If prostate cancer is in an early stage, is growing slowly, and treating the cancer would cause more problems than the disease itself, a doctor may recommend active surveillance or watchful waiting.
Active surveillance. Prostate cancer treatments may seriously affect a person's quality of life. These treatments can cause side effects, such as erectile dysfunction, which is when someone is unable to get and maintain an erection, and incontinence, which is when a person cannot control their urine flow or bowel function. In addition, many prostate cancers grow slowly and cause no symptoms or problems. For this reason, many men may consider delaying cancer treatment rather than starting treatment right away. This is called active surveillance. During active surveillance, the cancer is closely monitored for signs that it is worsening. If the cancer is found to be worsening, treatment will begin.
Watchful waiting may be an option for older men and those with other serious or life-threatening illnesses who are expected to live less than 5 years. With watchful waiting, routine PSA tests, DRE, and biopsies are not usually done. If the prostate cancer causes symptoms, such as pain or blockage of the urinary tract, then treatment may be recommended to relieve those symptoms.
•Surgery
Surgery involves the removal of the prostate and some surrounding lymph nodes during an operation. A surgical oncologist is a doctor who specializes in treating cancer using surgery. For prostate cancer, a urologist or urologic oncologist is the surgical oncologist involved in treatment. The type of surgery depends on the stage of the disease, the man’s overall health, and other factors.
• Radiation therapy is the use of high-energy rays to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time.
• Focal therapies
Focal therapies are less-invasive treatments that destroy small prostate tumors without treating the rest of the prostate gland. These treatments use heat, cold, and other methods to treat cancer, mostly for low-risk or intermediate-risk prostate cancer. Focal therapies are being studied in clinical trials. Most have not been approved as standard treatment options.
Cryosurgery, also called cryotherapy or cryoablation, is a type of focal therapy. It is the freezing of cancer cells with a metal probe inserted through a small incision in the area between the rectum and the scrotum, the skin sac that contains the testicles. It is not an established therapy or standard of care for men newly diagnosed with prostate cancer. Cryosurgery has not been compared with radical prostatectomy or radiation therapy, so doctors do not know if it is a comparable treatment option. Its effects on urinary and sexual function are also not well known.
High-intensity focused ultrasound (HIFU) is a heat-based type of focal therapy. During HIFU treatment, an ultrasound probe is inserted into the rectum and then sound waves are directed at cancerous parts of the prostate gland. This treatment is designed to destroy cancer cells while limiting damage to the rest of the prostate gland. The FDA approved HIFU for the treatment of prostate tissue in 2015. HIFU may be an attractive option for some people, but knowing who may benefit most from this treatment is still unknown. Similarly, HIFU should only be performed by a specialist with a lot of expertise. You will need to carefully discuss with your doctor if HIFU is the best treatment for you.
Disclaimer: All information in this site is intended for general information. It is not a substitute for medical advice from a health-care professional and is not intended to diagnose, treat, cure or prevent any disease. We only have access to and collect information that you voluntarily give us via email or other direct contact from you. We will not sell, rent, or otherwise disclose your information to any third-party. We will only use your information as necessary to respond to your requests. Read full disclaimer here.